Introduction
Inflammatory bowel disease (IBD), encompassing Crohn’s disease and ulcerative colitis, is a chronic condition that affects the digestive system. Characterized by inflammation of the digestive tract, IBD can cause a range of symptoms, including abdominal pain, diarrhea, fatigue, and malnutrition. While there is no cure for IBD, effective treatments can help manage symptoms and achieve remission.
Living with IBD can be challenging, both physically and emotionally. The unpredictable nature of the disease can disrupt daily life, making it difficult to plan and maintain a sense of normalcy. However, with proper management, a strong support system, and a resilient mindset, individuals with IBD can live fulfilling and healthy lives.
Understanding IBD: Delving into the Causes, Symptoms, and Types
IBD is an autoimmune disease, meaning that the body’s immune system mistakenly attacks healthy cells in the digestive tract. This inflammation leads to a range of symptoms, including:
- Abdominal pain and cramping
- Diarrhea, often bloody
- Fatigue
- Weight loss
- Anemia
- Fever
The severity of symptoms can vary from person to person and may fluctuate over time. Some individuals may experience periods of remission, where symptoms are minimal or absent, followed by flare-ups when symptoms worsen.

Crohn’s Disease: A Closer Look
Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus. It is characterized by inflammation that extends deep into the bowel wall, causing ulcerations and fissures. Symptoms of Crohn’s disease may include:
- Abdominal pain, often in the lower right abdomen
- Diarrhea, sometimes bloody
- Fatigue
- Weight loss
- Fever
- Mouth sores
- Fistulas (abnormal connections between organs or tissues)
- Anal abscesses
Ulcerative Colitis: Unraveling the Inflammatory Process
Ulcerative colitis affects only the large intestine (colon) and rectum. It is characterized by continuous inflammation that starts in the rectum and spreads upward along the colon. Symptoms of ulcerative colitis may include:
- Bloody diarrhea
- Abdominal pain, often in the lower left abdomen
- Urgency to defecate
- Fatigue
- Weight loss
- Fever
- Nighttime bowel movements
Management Strategies: Embracing Effective Treatment and Lifestyle Modifications
The primary goal of IBD treatment is to manage symptoms and achieve remission. Treatment options vary depending on the type and severity of IBD, but may include:
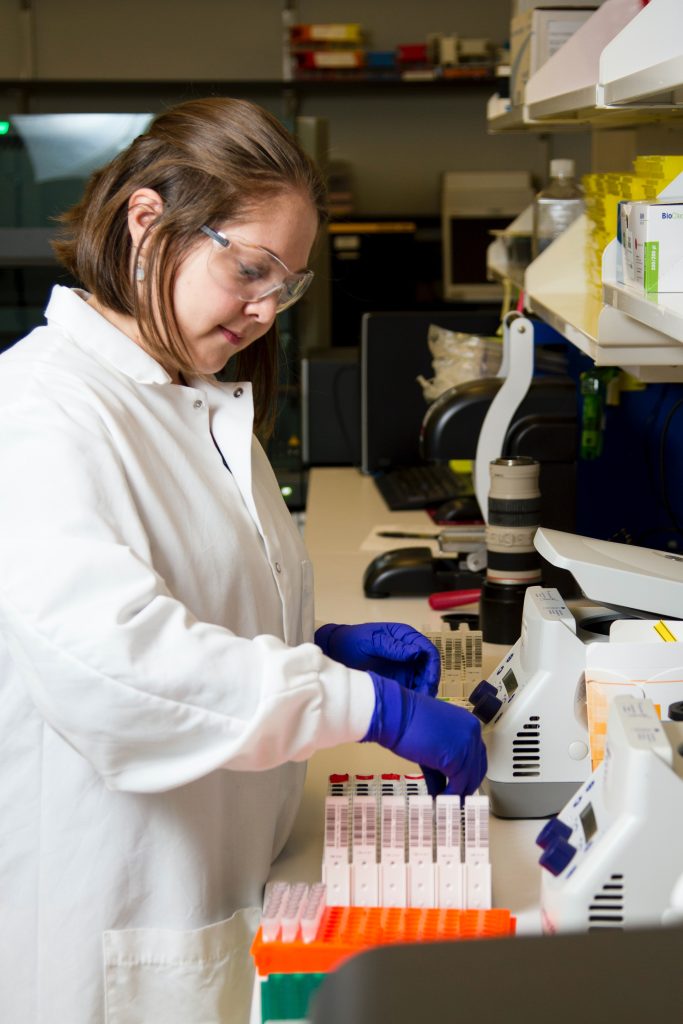
- Medication: A variety of medications can be used to reduce inflammation and control symptoms. These include anti-inflammatory drugs, immunosuppressants, and biologics.
- Diet: Dietary changes may help manage symptoms and improve overall health. Some individuals with IBD find that avoiding certain foods, such as dairy, gluten, or spicy foods, can reduce symptoms.
- Surgery: In some cases, surgery may be necessary to remove a damaged section of the digestive tract.
Lifestyle Modifications for Enhanced Well-being
Beyond medication and diet, lifestyle modifications can play a significant role in managing IBD and promoting overall well-being. These include:
- Stress Management: Chronic stress can worsen IBD symptoms. Practicing stress-reducing techniques such as yoga, meditation, or deep breathing can help improve symptoms and overall well-being.
- Sleep: Adequate sleep is crucial for physical and emotional health. Aim for 7-8 hours of quality sleep each night to support your body’s healing processes.
- Exercise: Regular physical activity can help reduce stress, improve mood, and strengthen the immune system. Engage in moderate-intensity exercise most days of the week.
- Smoking Cessation: Smoking can aggravate IBD symptoms and increase the risk of complications. Quitting smoking can significantly improve overall health.
Emotional Well-being: Navigating the Psychological Impact of IBD
Living with a chronic illness can take a toll on emotional well-being. Stress, anxiety, and depression are common among individuals with IBD. These emotional challenges can further impact physical health and make it more difficult to manage symptoms.
To foster resilience and emotional well-being, individuals with IBD can consider:
- Seeking support: Joining a support group or connecting with others who understand IBD can provide valuable emotional support and coping strategies.
- Talking to a therapist: A therapist can provide individual counseling to help manage stress, anxiety, and depression.
- Practicing self-care: Engaging in activities that promote relaxation and stress reduction, such as yoga, meditation, or spending time in nature, can significantly improve emotional well-being.
- Maintaining a positive outlook: Focusing on the positive aspects of life, despite the challenges of IBD, can help maintain a sense of hope and optimism.
Embracing Life with IBD: A Journey of Resilience, Hope, and Fulfillment
Despite the challenges, individuals with IBD can live fulfilling and healthy lives. By working closely with a healthcare team, managing symptoms effectively, prioritizing emotional well-being, and embracing a resilient mindset, individuals with IBD can achieve remission, maintain their independence, and pursue their goals.
A Call to Action: Embracing Advocacy and Community
Individuals with IBD can play a powerful role in advocating for themselves and others living with the disease. By sharing their experiences, raising awareness, and supporting research initiatives, individuals with IBD can help improve understanding, treatment options, and quality of life for all those affected by the disease.
In addition, connecting with the IBD community through support groups, online forums, and local organizations can provide invaluable support, information, and camaraderie. Sharing experiences, exchanging tips, and offering encouragement can foster a sense of belonging and empower individuals to navigate the challenges of IBD with strength and resilience.
Living with IBD is a journey, not a destination. It is about adapting, finding strength amid challenges, and embracing the many joys and possibilities that life has to offer.
Sources:
- PereraEssence, Thompson, J. M., AsmundsonGordon, J. G., El-GabalawyRenée, AfifiTracie, O., Sareen, J., & Bolton, S. (2021). Chronic pain: The Canadian Armed Forces members and Veterans mental health follow-up survey. Journal of Military, Veteran and Family Health, 7(S2), 29–42. https://doi.org/10.3138/jmvfh-2021-0051
- Lim, A., & Marcellus, L. (2023). Riding the wave: A grounded theory of transplant transition in adolescents and youth adults. Health Care Transitions, 1, 100019. https://doi.org/10.1016/j.hctj.2023.100019
- Ee, C., Thuraisingam, S., Pirotta, M., French, S., Xue, C. C., Teede, H., Kristoffersen, A. E., Sirois, F. M., Stub, T., Engler, J., Joos, S., Güthlin, C., Felenda, J., Beckmann, C., Stintzing, F. C., Evans, R., Brønfort, G., Keefe, D. F., Taberko, A., . . . He, Y. (2017). World Congress Integrative Medicine & Health 2017: Part one. BMC Complementary and Alternative Medicine, 17(S1). https://doi.org/10.1186/s12906-017-1782-4